Noticias

- Título: Philips expands interventional oncology portfolio with EmboGuide to see, reach and treat tumor lesions
- Fecha: 15-05-2014
- New live 3D image guidance tool enhances tumor embolization procedures on Philips’ interventional X-ray systems.
- Philips innovations detect more than twice as many tumor feeding arteries compared to standard DSA, while lesion detection is superior to standard DSA and now comparable to gold standard contrast-enhanced MRI [1,2].
Best, the Netherlands – Royal Philips (NYSE: PHG; AEX: PHIA) today announced the launch of EmboGuide, its latest innovation in interventional oncology, to treat difficult-to-reach tumors or tumors in patients who are deemed unsuitable for surgery.
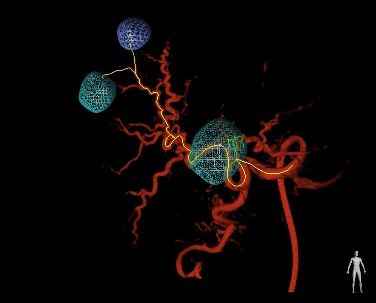
EmboGuide is a live 3D image guidance tool that supports the increasing number of minimally-invasive procedures. It is designed for use in conjunction with Philips’ interventional X-ray system to perform tumor embolization procedures. Such procedures involve blocking the arteries feeding a tumor to deprive it of nutrients and oxygen. They require the insertion of a catheter, which must be guided to the tumor site with the aid of live image-guidance.
Developed in collaboration with leading clinicians and partners such as BTG, an innovator in interventional oncology, EmboGuide addresses the need for an enhanced 3D imaging solution to make interventional oncology procedures more effective and easier to perform, and ultimately improve patient outcomes. It offers interventional radiologists the ability to visualize and characterize tumor lesions and plan and execute interventional procedures.
“Interventional oncology is a fast growing field that offers clinicians a viable treatment option for patients who are not suitable for surgical tumor removal,” said Gene Saragnese, CEO Imaging Systems at Philips Healthcare. “Together with our partners, we will leverage our combined expertise in image-guided interventions and therapies to accelerate this transformation from surgical procedures to minimally-invasive treatments in oncology.”
A specific example of a tumor embolization procedure is transarterial chemo-embolization (TACE), used for palliative treatment of liver tumors. It involves simultaneous local administration of chemotherapy and beads that block the arteries feeding the liver tumor.
“We can only treat what we see, yet the embolization of all blood vessels that feed the liver tumor lesion is key for an effective TACE procedure,” said Shiro Miyayama, MD, Department of Diagnostic Radiology, Fukuiken Saisekai Hospital, Japan. “EmboGuide’s live 3D image guidance helps to improve the technical success of the procedure, as it can automatically identify the small tumor-feeders that are difficult to detect with conventional 2D angiographic imaging methods.”
See - EmboGuide leverages the ultra-low X-ray dose settings of Philips’ AlluraClarity interventional X-ray system and the fast, high quality imaging of the abdomen of XperCT Dual. XperCT Dual’s enhanced imaging technique (multiphase cone beam CT) offers high quality 3D images of lesions, with proven detection accuracy superior to conventional 2D angiographic imaging. It offers clinicians a better view of the treatment targets for informed decision making while performing the procedure. XperCT Dual is comparable to MRI, which is considered to be the ‘gold standard’ [1,2].
Reach - EmboGuide helps to define the tumor lesions and features automatic identification of blood vessels that feed the lesions. It detects more than twice as many tumor feeding arteries compared to conventional imaging methods (Digital Subtraction Angiography (DSA) [1]. This allows interventional radiologists to optimize the catheter locations for embolization and plan a route to them. During the administration of the embolization agent, EmboGuide accurately superimposes the planning information onto the interventional X-ray system’s live images to monitor the treatment progress and determine its endpoint [3-5].Treat - “In the treatment of intermediate HCC, the integrated use of our embolic device with image guidance is vital for successful treatment,” said Mike Motion, BTG General Manager, Interventional Oncology. “As a leader in interventional oncology, we invest to improve the safety and efficacy of the procedure. Partnering with Philips has strengthened our ability to further develop this cohesive approach using DC Bead® and Philips’ EmboGuide with the ultimate objective of advancing interventional oncology.”
The launch of EmboGuide is a result of Philips’ global investment in Healthcare R&D, which amounted to a total of EUR 780 million in 2013. It highlights Philips’ commitment to interventional oncology - a rapidly developing market with a compound annual growth rate of around 15%.
Philips’ EmboGuide will be on display at the Asia-Pacific Congress of Cardiovascular and Interventional Radiology (APCCVIR) in Singapore from May 15 to 18. At the congress, Dr. Miyayama will share his experiences with EmboGuide in a scientific presentation titled ‘Lesion detection and feeding Vessel identification in HCC with XperCT Dual and EmboGuide’.
EmboGuide is currently not available in the USA.
References:[1] Identification of Small Hepatocellular Carcinoma and Tumor-feeding Branches with Cone-beam CT Guidance Technology during Transcatheter Arterial Chemoembolization; Miyayama et al.; Journal of Vascular and Interventional Radiology (April 2013); Volume 24, Issue 4; p. 501-508.
[2] Comparing the Detectability of Hepatocellular Carcinoma by C-Arm Dual-Phase Cone-Beam Computed Tomography During Hepatic Arteriography With Conventional Contrast-Enhanced Magnetic Resonance Imaging; Loffroy et al.; CardioVascular and Interventional Radiology (February 2012); Volume 35, Issue 1; p. 97-104.
[3] Intraprocedural C-Arm Dual-Phase Cone-Beam CT: Can It Be Used to Predict Short-term Response to TACE with Drug-eluting Beads in Patients with Hepatocellular Carcinoma?; Loffroy et al.; Radiology (February 2013); Volume 266, Number 2; p. 636-648.
[4] Comparison of Local Control in Transcatheter Arterial Chemoembolization of Hepatocellular Carcinoma <6 cm With or Without Intraprocedural Monitoring of the Embolized Area Using Cone-Beam Computed Tomography; Miyayama et al.; CardioVascular and Interventional Radiology; (April 2014); Volume 37, Issue 2; p. 388-395.
[5] Transarterial Chemoembolization with Drug-eluting Beads in Hepatocellular Carcinoma: Usefulness of Contrast Saturation Features on Cone-Beam Computed Tomography Imaging for Predicting Short-term Tumor Response; Suk et al.; Journal of Vascular and Interventional Radiology (April 2013); Volume 24, Issue 4; p.483-489.- Fuente: endovascular.es





